II. Introduction: The Unique Legal Calculus of the NICU
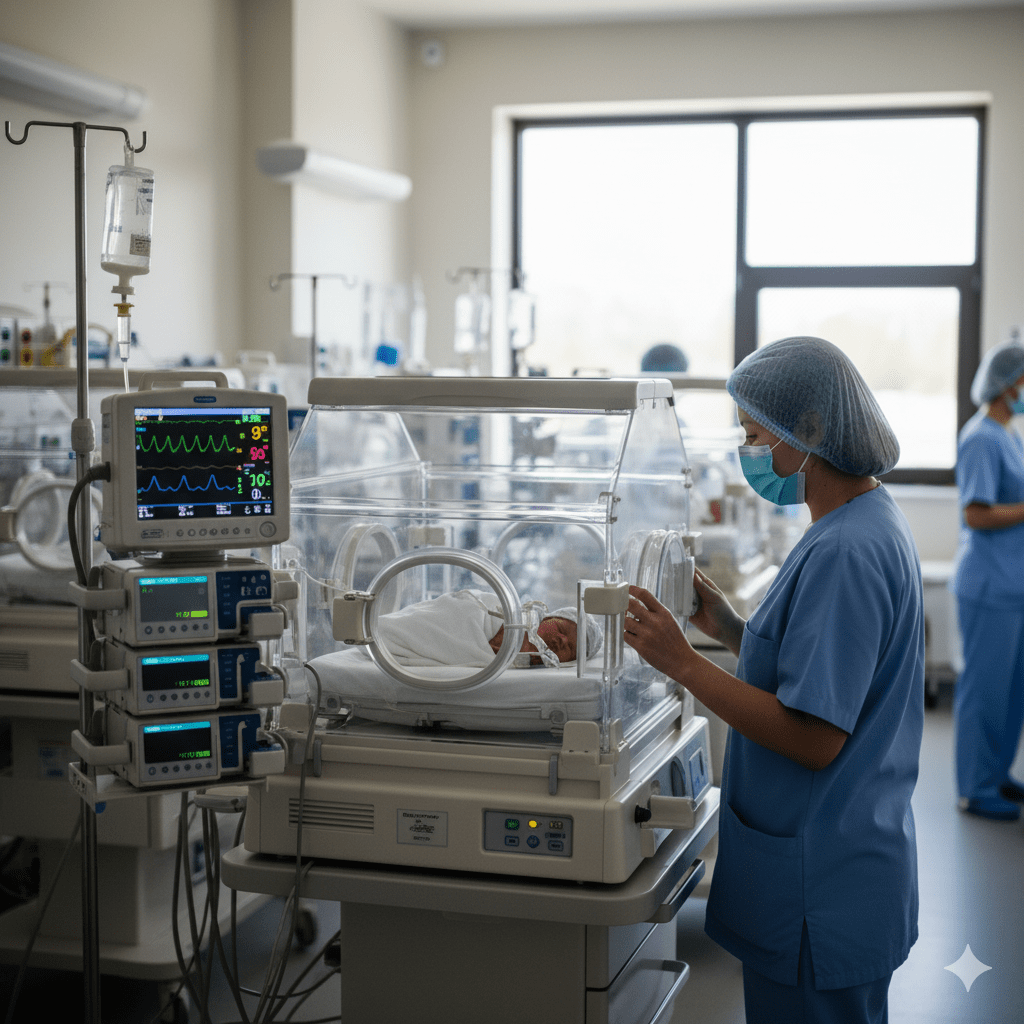
The Neonatal Intensive Care Unit (NICU) is medicine’s most challenging arena. A “bad outcome” is often the tragic, yet expected, natural sequelae of prematurity. For attorneys and physicians, the legal calculus is unique: every NICU medical malpractice case starts with the defense shield that the infant was inherently fragile.
To prevail in litigation, the plaintiff must prove that the provider not only failed the Standard of Care (SOC) but failed it in a way that actively removed the infant’s already slim chance of a healthy outcome. The question becomes: “Would the outcome have been different if the SOC were met?” As an attorney I frequently consult with once remarked, “Causation is the goal line prevent defense for these cases.” Your consulting pediatric medical malpractice expert is essential to separate the inevitable risks of a premature birth from preventable clinical negligence.
II. Core Pathology and the Diagnostic Conundrum
The defense often argues that the infant’s injury (such as cerebral palsy or chronic lung disease) stems from the underlying illness. Attorneys must preemptively counter this argument by focusing on process-driven failures—the timing and efficiency of life-saving interventions.
One of the greatest hazards is Neonatal Sepsis. The clinical signs—lethargy, subtle temperature instability, or poor feeding—are often non-specific and easily mistaken for general prematurity issues. The SOC, however, demands extreme vigilance and often prophylactic treatment based on high suspicion. The case hinges entirely on the timing and completeness of the sepsis workup (blood labs and cultures), as well as the immediate initiation of broad-spectrum IV antibiotics.
III. Deep Dive: Necrotizing Enterocolitis (NEC)—The Documentation Trap
Necrotizing Enterocolitis (NEC), the devastating death of intestinal tissue, is a prime example of a process-driven liability. NEC is a leading cause of morbidity and mortality in premature infants, and the primary risk factor is enteral feeding.
The key Standard of Care here involves strict, gradual advancement of feedings and hyper-vigilance for early signs. The legal pitfall often turns on the quality of documentation:
- Breach 1 (Feeding Protocol Absence): Was a predetermined, evidence-based feeding protocol absent, or was the existing protocol incorrectly applied, causing overfeeding? This represents a systemic, quantifiable breach of the SOC.
- Breach 2 (Failure to Act on Signs): Were subtle signs like abdominal distention or guaiac-positive stools documented by nursing staff but ignored or dismissed by the physician during rounding? This highlights a dangerous communication or supervisory failure.
The plaintiff must show the physician failed to order an abdominal X-ray (KUB) at the first vague sign of trouble.
IV. Proving the “Aggravated” Standard of Care Breach
NICU malpractice cases are the high-stakes poker of pediatric medical malpractice. Damages frequently reach the millions. Yet, the difficulty in litigating these cases increases by orders of magnitude. For both sides, understanding that the fragility of the NICU patient actually raises the SOC is paramount.
For physicians, the defense rests entirely on providing rigorous documentation showing that you were performing serial exams and actively ruling out life-threatening diagnoses at every single shift change.
For attorneys, the causation hurdle is immense. You must use a pediatric medical malpractice expert to testify that a specific, timely intervention—such as ordering that single X-ray, or initiating antibiotics four hours earlier—would have likely prevented the catastrophic outcome. Without this strong causative link, the defense will successfully argue the inevitable consequences of prematurity.
Engaging a consultant early ensures you isolate the precise timeline where inevitable risk gave way to preventable negligence.
Leave a comment